“He paid the ultimate price,” Wind said. “He saved my life.”
By Samantha Stetzer
Kelly Wind was sitting in the imaging lab area of Winona Health in late 2014, when she was told there was early cancer forming in her breast.
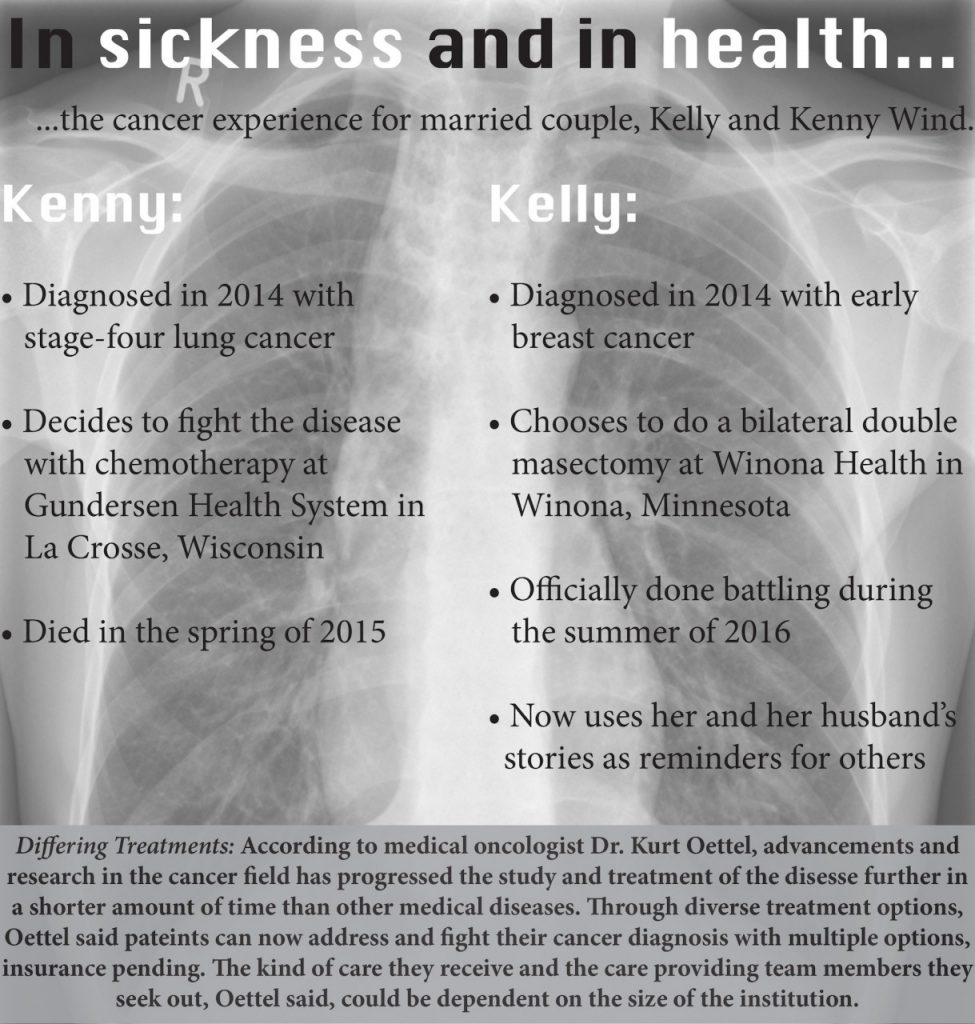
Her husband of almost 25 years, Kenny Wind, had been diagnosed with stage four-lung cancer months earlier. His prognosis was bleak, Kelly said, but he was fighting, despite the low chances for survival.
She said his diagnosis had inspired her to get a routine mammogram. That mammogram led a radiologist to find something suspicious on her scans. After tests and ultrasounds, she officially had a cancer diagnosis.
With her disease identified, Kelly said the fear and weight of the word cancer was setting in, but a voice cut through her doubt.
“Hey, you are not going to die from this, do you hear me,” a nurse named Heather said, Kelly recalled.
Thus began a year and a half relationship between Kelly and her cancer care team at Winona Health.

Between Winona Health in Winona, Minnesota, and Gundersen Health System in La Crosse, Wisconsin, Kelly said she and her husband could choose the types of cancer treatments they preferred, and depending on their choices, they met with a series of providers and caregivers who helped the disease.
The Commission on Cancer accredits both of these hospitals as cancer centers, according to each of the organizations. Gundersen Health System is also accredited by the American College of Radiology.
Kelly said she believes the care she received at Winona Health was just right for her. She made relationships, partnerships and friendships with everyone who cared for her. She said she felt the staff was personable.
“My journey was just amazing,” Kelly said.
She created bonds with the receptionist, the nurses and her surgeons, as she went through a double mastectomy, meaning both of her breast tissues were removed. Later, eventually replaced them with new breasts, making the recovery process from cancer last a year and a half.
A double mastectomy was just one option Kelly said she had. According to Sandy Gruzynski, Winona Health’s patient navigator, while Winona Health cannot offer chemotherapy or radiation treatments right now, their partnerships with the Mayo Clinic Network, headquartered in Rochester, Minnesota, and Gundersen can help patients find the treatment that best fits how they wish to fight the disease.
When the word cancer is spoken as a diagnosis to a patient, Gruzynski is the first person a provider calls. Kelly said she remembers working with Gruzynski to find the best treatment for her disease, describing her as a “warrior” patients.
Gruzynski said she lists options for patients, such as treatments or goals for finishing out the rest of their illness is terminal.
For patients with breast cancer such as Kelly, there are many treatments options because the disease has been heavily researched, Gruzynski said.
Within treatments, such as chemotherapy, Gundersen Health System Medical Oncologist Dr. Kurt Oettel said there can be different aspects to each therapy, which each patient has to consider when choosing a plan for treatment.
“Chemotherapy is like saying ‘I drive a car’,” Oettel said. Simply stating this fact about a vehicle does not give the full story as to what kind of car a person drives, much like how having a patient choosing a chemotherapy track is not uniform for all cancer patients.
Chemotherapy is one example of the progress and research done about cancer treatments that has made cancer research a rapidly growing field, Oettel said.
At conferences, presentations frequently highlight new techniques and treatments for patients, Oettel added, highlighting how this changes the field of cancer dramatically over short periods of time.
“It’s a fast-changing field,” Oettel said. “What’s presented at that meeting… the standard of care just changed over night.”
Oettel said he has had patients whose treatment plans changed within two months, due to advancements in care.
“Now patients live much longer,” Oettel said.
When Kelly was given her options to fight the cancer, she said she was given multiple options, including a lumpectomy, where just the cancerous mass in the breast is removed. There was also chemotherapy, where the disease could be attacked without surgery.
Kelly said she feared the cancer could appear again, and she said she was ready to say goodbye to her breasts, especially if it meant she would have a better chance of surviving.
She told the care team at Winona Health she was “done with them.”
“Take it. I’m done,” Kelly recalled saying with a laugh.
Kelly said her treatment choice was easy: it gave her the best chance to live. Her mastectomy was the only way she said she could ensure she could be there for her four kids and five grandchildren, especially with her husband’s failing health.
She was not going to let them lose another parent in such a short amount of time, Kelly said.
Her kids had just accepted the fact their father was going to die, Kelly added, but her eldest daughter was struggling with the possibility that her mom could die too. As tears welled in her daughter’s eyes, Kelly recalled how she took the advice of the nurse in imaging at Winona Health.
“I told her I was going to beat this, Kelly said.
While Kelly was fighting at Winona Health, her husband was being treated in La Crosse, Wisconsin, at Gundersen Health System with weekly treatments. Kelly said she had to continue her work at Riverstar Inc., where she unloads boxes, even if it meant missing some of his appointments, so she could pay the bills.
At Gundersen, Kelly said Kenny’s experience was more rigid, adding she saw how he was more of a number than a person.
That form of treatment was just right for Kenny, Kelly said. He appreciated the atmosphere, she added, especially in a place where providers have to care for a large variety of cancers and people.
“They weed out so many people… an entire floor of chemo,” Kelly said. “It was more comfortable for him.”
According to Oettel, the reason Kenny and Kelly might have felt like his treatment was differed from Winona Health’s is because Gundersen Health System is comprised of a large network of cancer providers all working to provide care to one patient through many options available at the hospital, such as chemotherapy and radiation.
Oettel explained how, unlike the process of treating a condition like heart disease, where one specialist is needed, the process a patient goes through when they are diagnosed with cancer involves several specialists helping each patient with certain steps in their cancer treatment process. Oettel said he is typically the doctor patients see after they have surgery to decide what steps are next, but there are other doctors and providers, such as the surgeons or radiologists, who have already been providing care to patients.
Since Gundersen has the capability to treat cancer through surgery, radiation and chemotherapy, Oettel said there are many caregivers and providers available to patients.
He added insurance availability is one of the main reasons patients make the decisions they do regarding the care they receive. Depending on their insurance, a patient can be limited with their choices for treatment and where they choose to be treated, Oettel explained.
At Winona Health, Gruzynski said she helps guide patients through their insurance process. She often helps decipher jargon within patients’ policies to help them decide which course of action to take and where to take it.
“Right now, it’s really an insurance-driven world,” Oettel said, adding doctors and caregivers should effectively explain to a patient the options at a facility based around a patient’s insurance.
With the constantly changing future of provider care, Oettel said he does not necessarily believe in the “holy grail cure” for all cancers but can foresee a time when cancer becomes a chronic illness like HIV or diabetes.
He added being able to utilize new treatments and options for patients to get into remission can be a great feeling for someone like him who spends his career trying to heal everyone he sees.
“That’s very rewarding to say ‘you no longer need to see me,’” Oettel said.
In spite of advancements in treatments and technologies, Oettel said he has to anticipate he will not cure 50 percent of his patients. He added working with dying patients can be a worthwhile part of his job.

For Kenny, remission never came. He died in the spring of 2015, just before he and his wife would celebrate their 25th wedding anniversary, according Kelly. In the summer of 2016, Kelly said she was officially done fighting her cancer.
After one and a half years of and with a drug prescription to help reduce her risk of getting the disease again, Kelly said there is now 98 percent chance her cancer will never come back. She said she uses her husband’s story and how it motivated her to get a check up as a constant reminder to her friends and family, often reminding the women in her life to get mammograms.
Looking back at where she was that winter day in 2014, Kelly said she credits her husband for making sure their children still have a parent today.
“He paid the ultimate price,” Wind said. “He saved my life.”